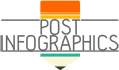
With personal finances, paying for medical care with your cash on hand is frustrating, especially when you have health insurance. The Affordable Care Act requires insurance companies to cover mental medical management, such as transcranial magnetic stimulation. But the coverage and approval differ for each provider.
Does insurance cover TMS treatment?
Medical requirements must be cited for treatments in order for the insurance provider to pay for them. It should meet the criteria listed below for TMS therapy:
- would be seeking treatment for covered illness like Major Depressive Disorder.
- tried talking to a psychotherapist to help with symptoms, but there wasn’t much of an improvement.
- possess a minimum of two verified antidepressant drug studies conducted at an acceptable dose and for the recommended duration.
Ask your provider for information on the specific criteria.
Will Medicaid and Medicare cover TMS therapy?
Each state has different coverage standards. It also depends on your individual plan and capacity to comply. Medicare will pay for up to 80% of the medical care. Make sure your annual deductible is met. You can determine how much you’ll have to pay after the insurance company has done its part by asking these questions.
- Would the Medicaid and Medicare-approved reimbursement amount be accepted as full payment by your treatment provider?
- Has your Medicaid/Medicare-approved physician diagnosed you with MDD?
- Have you used medication to treat your MDD ineffectively? Do any of the prescribed medications cause you harm?
In-Network vs. Out-Of-Network Coverage
In-network providers have set a pricing with a coordinated reimbursement process with your insurance provider. This is more convenient on your part compared to out-of-network TMS providers. It’s possible that you’ll have to pay for the procedure up front and ask your insurance provider for reimbursement afterwards. To avoid any unexpected payments and paperwork, check with your insurance provider on how they will approach it.
Disqualifying Situations
Sometimes, even if the treatment is proven to be medically necessary, your insurance provider will not cover it. It could be any of these reasons:
- had seizures or seizure disorder in the past
- have medical devices or objects in your body that are magnetic-sensitive
- have a history of memory disorder diagnosis
- have an continuous problem with substance usage
Increasing Your Possibility for Treatment Coverage
The insurance company has the final decision to cover the expenses for your TMS therapy, but there are several things you can do to help improve your chances of reimbursement for your treatment.
1. Get Educated
If there are disqualifying situations, recognize them and see if it is short-term. Don’t give up too soon since your insurance might cover your treatment when the circumstances change.
2. Follow the Specified Treatment Programs
Even with draining symptoms, toughen up and follow the prescribed treatment. This will prove to the insurance company of your situation and motivation to get better.
3. Keep Correct Records
Document your medical history of past treatments. This will help your doctors understand your experiences.
Insurances should cover TMS therapy, but with a few exceptions. Learn about these conditions and the standard needed to be eligible for coverage. If you are having a hard time, reach out to someone that can assist you in navigating the potential issues and securing coverage.
source: https://neurostimtms.com/tms-therapy-will-insurance-cover-treatments/
Comments
Download this infographic.